Introduction
In New York City and around the world, diet-related chronic diseases are rapidly becoming the leading cause of premature death, preventable illnesses, and disability. Conditions such as diabetes, cardiovascular diseases, hypertension and some forms of cancer also impose a burden of suffering on individuals and families, costs on our health care systems, and lost productivity to the economy. Globally, diet-related chronic diseases are also a leading cause of the health inequities between the better off and the poor and, in New York City and the United States, between whites and people of color.
On Thursday, September 27, the Third United Nations High Level Meeting on Non-Communicable Diseases takes place in New York City. Its goal is to assess global progress in reducing non-communicable diseases (NCDs), the public health term for chronic diseases, and to make recommendations for governments, businesses and civil society to act to prevent and manage these conditions. After the first UN General Assembly Global NCD meeting in 2011, international organizations set the goal of a 25% reduction in premature mortality from noncommunicable diseases by 2025.

Source: WHO
A 2010 World Health Organization (WHO) report meeting identified four main risk factors for NCDs: unhealthy diets, tobacco use, alcohol use and sedentary behavior.1 Progress in preventing NCDs, observed the WHO, required not simply changing individual behavior but enlisting all sectors of society to act to reduce exposure to these risk factors.
No single cause explains the rapid growth of NCDs around the world and no single policy will reverse the epidemics of diet, tobacco, alcohol and inactivity-related diseases. Clearly, individual behavior; local, national and global public policies; demographic shifts and changes in the global economy all contribute. But a mounting body of evidence shows that the practices of the food, alcohol and tobacco industries play a significant role in the growing NCD burden.2 By considering the commercial practices of the food industry as modifiable social determinants of health, public health researchers can identify new opportunities for preventing NCDs.
This policy brief summarizes what is known about the impact of food industry practices on diet-related NCDs and describes some of the actions government, civil society and business have taken to prevent these conditions since the 2011 UN meeting. Finally, it examines how in the coming years New York City can learn from and teach others from around the world how to change the food industry practices that contribute to diet-related NCDs.

Source: spulsa.info
How do food industry practices contribute to NCDs?
Both the business practices and the political practices of the food industry contribute to diabetes, cardiovascular diseases, hypertension and some forms of cancer. Taking in more calories than an individual burns and the associated increases in overweight and obesity are a primary link between diet and ill health, but not the only pathway. Foods high in sugar, salt and some kinds of fat, and foods that are highly processed (or ultra-processed) are more associated with NCDs than healthier foods. These ultra-processed products are claiming an ever larger portion of global caloric consumption.3 Some evidence shows that unhealthy diets also contribute to inflammation, changes in gut microbiota and other processes that can cause or exacerbate NCDs.4
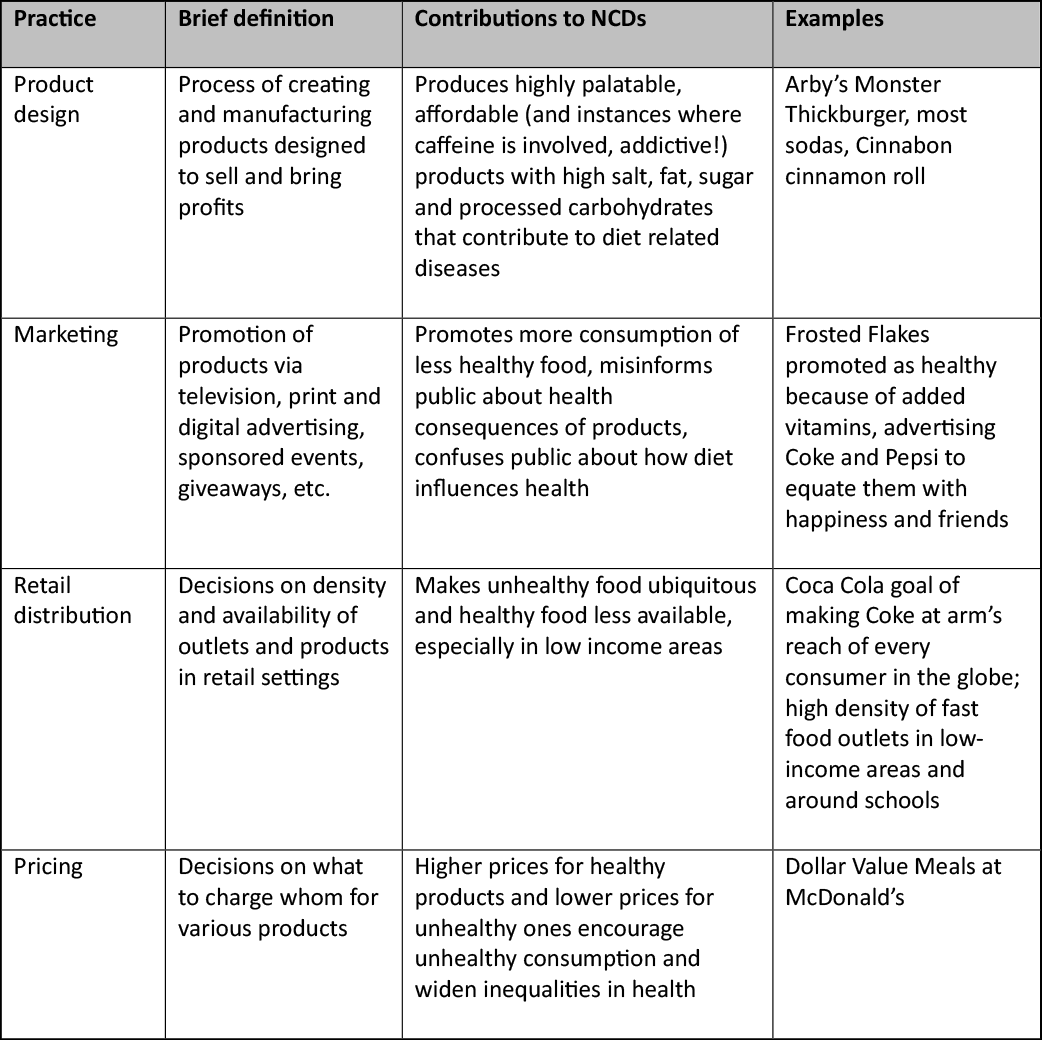
Table 1. Food Industry Business Practices
Food industry business practices include product design, marketing, distribution and pricing. Companies carry out these activities to advance business goals such as increased profits and increased market share, even when these practices may have harmful health consequences. As shown in the table, each of these practices has been shown to contribute to diet-related diseases.
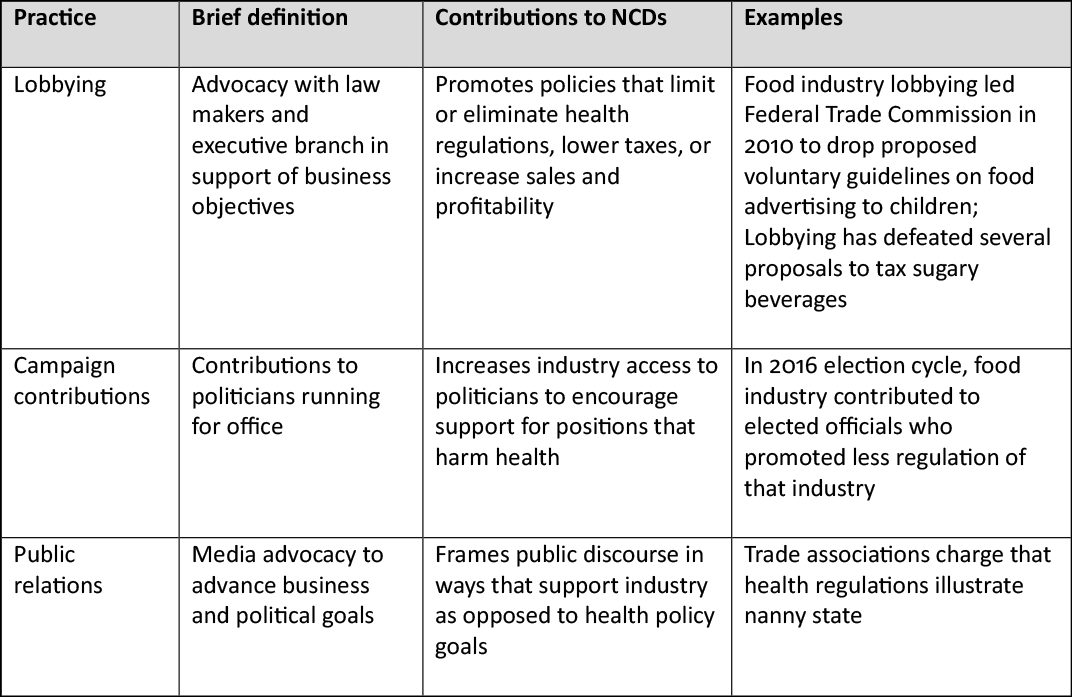
Table 2. Food Industry Political Practices
In addition to the business practices described above, food industry political practices compound their contribution to NCDs. Food industry political practices seek to create a social, political and economic climate in which food businesses can pursue their business objectives without interference from government or consumers and with less risk to growth and profitability, as shown in the table below. Common goals of the political practices are to decrease corporate taxes; defeat, delay or weaken regulations; enhance the image or credibility of the corporation in the face of criticism; win support from other powerful players; or win passage of favorable trade policies. The vast financial and political resources of the global food industry compared to those available to public health and civil society advocacy groups ensure that industry voices play a disproportionate role in setting policy.
How have global changes in the food industry increased the risk of diet-related disease?
Several changes in the global food industry in the last few decades have contributed to the rise in NCDs. First, the high and rapidly increasing levels of concentration in the agriculture, food production and food retail businesses reinforce industrial food and farming models that promote the highly processed foods most associated with diet-related diseases.6 Transnational corporations like Nestle, Unilever and Kraft develop global markets for their products and have the power to bring their products to billions of consumers. They also push smaller competitors out of business or buy them up, reducing competition on price and quality of food. These changes also exacerbate the food sector’s social and environmental fallout and aggravate existing power imbalances.7 New technologies allow these giant companies to process ever more food products and invest in marketing them to more sectors of the population.
In the past few decades, as food corporations grew larger and more global, they claimed powers that had previously been in the hands of government. Food and other companies gained control over setting global trade policies, self-regulate their practices, sponsor and interpret scientific research and educate the public about food. In each of these tasks, corporations have consistently set profitability not health and the prevention of disease as their priority.
Compared to 50 years ago, the world’s largest food companies have a bigger voice in shaping the world’s dietary choices, produce more of the calories that the world consumes, and reach inside the minds of more consumers. Increasingly, ultra-processed foods can be shipped anywhere in the world, sit on shelves for months, and be marketed to satisfy deep emotional longings (“Open happiness!”). These characteristics are what make them better generators of income than healthier products. Despite occasional health rhetoric and use of health claims to market products, few global food companies want to reduce consumption of their most profitable products— and it is these same products that also happen to be a primary cause of NCDs.
What actions have been taken to modify harmful food industry practices?
Around the world, governments and civil society groups have advocated for policies and programs that can reduce the disease burden of food. What have been some of their successes? In a 2011 report, the World Health Organization identified “Best Buys” in policies to reduce diet-related diseases.8 Other recent reports have proposed other evidence-based or promising policies.9 Several of these target harmful practices of the food industry:
- Reduce salt intake in food10
- Replace trans-fat with polyunsaturated fat11
- Tax sugar or sugary beverages12
- Mandate warning labels on unhealthy products such as soda13
- Require front-of-pack labels14
- Restrict marketing of breast milk substitutes15
Source: paho.org16
Other promising policies which have been less evaluated to date include those that restrict advertisement of unhealthy foods, especially to children;17 public countermarketing campaigns;18 and stricter rules and more vigorous enforcement of anti-monopoly rules.19
Some public health researchers advocate public private partnerships, in which corporations, government and civil society groups develop and enforce often voluntary guidelines.20 In the United Kingdom, for example, “Responsibility Deals” brought together government, businesses and advocates to set voluntary standards for improving the healthfulness of food. The few empirical studies of the Responsibility Deal and other such partnerships have not shown significant impact.21
What can New York City learn from and teach others about modifying harmful business practices?
New York City has played a leading role in developing municipal strategies to reduce corporate practices that contribute to diet-related NCDs.22 It has:
- Imposed a ban on commercial use of trans fat which served as a model for other cities and state and in the United States as a whole;
- Used a variety of strategies to encourage food manufacturers to reduce the salt in processed foods and to educate consumers about the dangers of excess salt;
- Led public education campaigns to encourage people to drink less sugary beverages and more tap water;
- Required chain restaurants to disclose calorie counts on menus;
- Established food standards that set limits on sugar, salt and unhealthy fats in school food and other institutional food programs.
- The city also sought but failed to limit the portion size of sugary beverages.
As the UN, the World Health Organization, international health organizations and others consider strategies to prevent diet-related NCDs, what strategies might help to further reduce food-industry practices that contribute to diet-related disease?
Source: nyc.gov
Next steps?
To achieve the goal of reducing premature mortality from diet-related diseases by 2025 will require significant acceleration of policy change. How can public health and nutrition professionals, food justice advocates and others contribute to the achievement of this target? We suggest four broad approaches actions that could help New York City, the United States and other nations to move in the right direction.
Strengthen public oversight of the food sector.
As the nutritionist Marion Nestle has observed, the message from the food industry will always be to eat more, not eat less.23 As long as high fat, sugar and salt ultraprocessed foods are their most profitable products, the food industry is unlikely to play a constructive role in changing food practices. Only government has the mandate and resources to make protecting public health a priority. Civil society groups can also play a useful role in asserting the rights of communities to create food policies that promote health rather than disease. By strengthening the role of the public sector to make public food– institutional food, restaurant food, food available in public benefit programs — healthier and more affordable, public policy can create an alternative to a commercial food system that values profits over health.
Similarly, by using existing mandates and resources, local, regional and national governments can implement “Best Buys” more systematically. They can tax sugary beverages and other unhealthy products, limit salt and unhealthy fats in processed food, require warning labels and useful reader-friendly nutrition labels on food products, and limit deceptive or manipulative food advertising, especially to children.
To reduce the political power of the food industry to block public health measures, governments can put limits on lobbying and campaign contributions, close the revolving door between industry and government, strengthen regulation of unsafe and unhealthy food, reject additional corporate tax breaks, make health a priority in trade agreements and set rules that minimize corporate manipulation of scientific research.
Finding ways to strengthen public oversight of the food industry is not so difficult. What is hard is for elected officials to find the will to stand up to industry resistance. By building constituencies that can demand that our elected officials resist industry pressure and support those who do, public health and nutrition professionals, food advocates and ordinary citizens can begin to create the foundation for achieving the WHO goal of 25% reduction in premature mortality from NCDs by 2025.
Provoke dialogue and debate on proper roles for government, food industry, communities and individuals in setting food policy.
In the last few decades, the food industry has monopolized public understanding of food, spending tens of billions more on shaping people’s food choices than public organizations. To balance this discussion, public health departments, nutritionists, community organizations and others need to encourage public discussion of these questions:
Who do you trust more to look after the nutritional well-being of your children and family—the food industry or public health authorities? If a globalized food industry requires oversight, is it the “nanny state” or the “nanny corporation” that will do a better job?
Should corporations be allowed to advertise directly to children? How can we balance the rights of corporations to make a profit with the rights of parents to protect their children and family’s health?
What roles should our schools play in educating children about food and eating? Should schools teach children how to detect and resist false, misleading or manipulative food advertising?
Use the powers of municipal government.
This includes zoning laws, public procurement, and regulation of food retail and restaurant businesses to encourage food industry practices that support health and discourage harmful practices. For example, zoning laws can be used to limit the density of unhealthy food outlets, procurement rules can help to improve the healthfulness of school food and other institutional food and retail policies can encourage developers to locate food stores that make providing healthy affordable food in redeveloped communities a priority.
Look for long term as well as short term wins in policies to reduce harmful food industry practices.
Short-term and easy victories are important and set the stage for more significant changes. But many elected officials always choose modest short-term goals, even when the evidence shows that such strategies will have at best a small impact on reducing diet-related disease. By insisting that the only viable policy options are those that can be won in the next budget or electoral cycle or the next legislative session, elected officials can overlook the deeper more significant changes needed to improve health and diets. After all, it took more than 50 years of scientific research, advocacy and litigation to impose significant public controls on the tobacco industry.
Of note, during the time that New York State rejected a soda tax and New York City lost its effort to limit the portion size of soda containers, soda consumption in New York City fell by daily soda consumption among New York City adults fell from 36% in 2007 to 24% in 2015. Raising health issues, even when the campaigns lose the first several times, can itself lead to behavioral changes. Public health advocates can help to bring about real improvements in diet-related disease by insisting that policies like restricting food advertising to children, limiting concentration within the food industry, and creating subsidized healthy-food restaurants are worth pursuing, even if they are heavy lifts in today’s political climate.
In the twentieth century, public campaigns to change food industry practices led to dramatic improvements in food safety, nutrition and population health.24 As the burden of diet-related NCDs grows, setting food policies that can reduce harmful food industry practices is a key priority.
Nicholas Freudenberg is Distinguished Professor of Public Health at the CUNY Graduate School of Public Health and Health Policy and Director of the CUNY Urban Food Policy Institute. His most recent book is Lethal but Legal Corporations, Consumption and Protecting Public Health. (Oxford University Press, 2014 and 2016 in paperback).
References
1. Global status report on noncommunicable diseases 2010. Geneva, World Health Organization, 2011.
2. See for example: Collin J, Hill SE, Eltanani MK, Plotnikova E, Ralston R, Smith KE. Can public health reconcile profits and pandemics? An analysis of attitudes to commercial sector engagement in health policy and research. PlOS ONE. 2017;12(9):e0182612. McKee M, Stuckler D. Responding to the Corporate and Commercial Determinants of Health. American Journal of Public Health. 2018 Sep(0):e1-4. Mialon M, Swinburn B, Sacks G. A proposed approach to systematically identify and monitor the corporate political activity of the food industry with respect to public health using publicly available information. Obesity Reviews. 2015 ;16(7):519-30. Allen, L. and Feigl, A.B., 2016. Reframing non-communicable diseases as socially transmitted conditions. The Lancet. 2017(5) e644-646.
3. See for example: Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra‐processed products are becoming dominant in the global food system. Obesity Reviews. 2013;14:21-8. Moreira PV, Baraldi LG, Moubarac JC, Monteiro CA, Newton A, Capewell S, O’Flaherty M. Comparing different policy scenarios to reduce the consumption of ultra-processed foods in UK: impact on cardiovascular disease mortality using a modelling approach. PLOS ONE. 2015;10(2):e0118353. Steele EM, Popkin BM, Swinburn B, Monteiro CA. The share of ultra-processed foods and the overall nutritional quality of diets in the US: evidence from a nationally representative cross-sectional study. Population Health Metrics. 2017;15(1):6.
4. Zinöcker MK, Lindseth IA. The Western Diet–Microbiome-Host Interaction and Its Role in Metabolic Disease. Nutrients. 2018;10(3):365.
5. Clark SE, Hawkes C, Murphy SM, Hansen-Kuhn KA, Wallinga D. Exporting obesity: US farm and trade policy and the transformation of the Mexican consumer food environment. Int J Occup Environ Health. 2012;18(1):53-65.
6. Mooney P. Too big to feed: Exploring the impacts of mega-mergers, consolidation and concentration of power in the agri-food sector. IPES-Food. 2017.
7. See for example: Kraak VA, Liverman CT, Koplan JP, editors. Preventing childhood obesity: health in the balance. National Academies Press; 2005. Mensah GA, Goodman RA, Zaza S, Moulton AD, Kocher PL, Dietz WH, Pechacek TF, Marks JS. Law as a tool for preventing chronic diseases: expanding the spectrum of effective public health strategies. Preventing Chronic Disease. 2004;1(1). Hawkes C, Smith TG, Jewell J, Wardle J, Hammond RA, Friel S, Thow AM, Kain J. Smart food policies for obesity prevention. The Lancet. 2015 Jun 13;385(9985):2410-21. Gittelsohn J, Trude ACB, Kim H. Pricing Strategies to Encourage Availability, Purchase, and Consumption of Healthy Foods and Beverages: A Systematic Review. Prev Chronic Dis 2017;14:170213
8. World Health Organization, World Economic Forum. From burden to “best buys”: reducing the economic impact of NCDs in low- and middle-income countries. Geneva: World Health Organization, 2011.
9. See for example: Kraak VA, Liverman CT, Koplan JP, editors. Preventing childhood obesity: health in the balance. National Academies Press; 2005. Mensah GA, Goodman RA, Zaza S, Moulton AD, Kocher PL, Dietz WH, Pechacek TF, Marks JS. Law as a tool for preventing chronic diseases: expanding the spectrum of effective public health strategies. Preventing Chronic Disease. 2004;1(1). Hawkes C, Smith TG, Jewell J, Wardle J, Hammond RA, Friel S, Thow AM, Kain J. Smart food policies for obesity prevention. The Lancet. 2015 Jun 13;385(9985):2410-21. Gittelsohn J, Trude ACB, Kim H. Pricing Strategies to Encourage Availability, Purchase, and Consumption of Healthy Foods and Beverages: A Systematic Review. Prev Chronic Dis 2017;14:170213
10. Jaenke R, Barzi F, McMahon E, Webster J, Brimblecombe J. Consumer acceptance of reformulated food products: A systematic review and meta-analysis of salt-reduced foods. Critical Reviews in Food Science and Nutrition. 2017 Nov 2;57(16):3357-72.
11. Downs SM, Bloem MZ, Zheng M, Catterall E, Thomas B, Veerman L, Wu JH. The impact of policies to reduce trans fat consumption: A systematic review of the evidence. Current Developments in Nutrition. 2017;1(12):cdn-117.
12. Roache S, Gostin L. The untapped power of soda taxes: incentivizing consumers, generating revenue, and altering corporate behavior. Int J Health Policy Manag. 2017;6(9):489–493.
13. Lee BY, Ferguson MC, Hertenstein DL, Adam A, Zenkov E, Wang PI, Wong MS, Gittelsohn J, Mui Y, Brown ST. Simulating the Impact of Sugar-Sweetened Beverage Warning Labels in Three Cities. Am J Prev Med. 2018 Feb;54(2):197-204. doi: 10.1016/j.amepre.2017.11.003.
14. Nestle M. Public health implications of front-of-package labels. American Journal of Public Health. 2018; 108(3):320.
15. Munn AC, Newman SD, Mueller M, Phillips SM, Taylor SN. The impact in the United States of the baby-friendly hospital initiative on early infant health and breastfeeding outcomes. Breastfeeding Medicine. 2016 Jun 1;11(5):222-30.
16. World Health Organization, 2017. Updated Appendix 3 to the Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013-2020.
17. Whalen R, Harrold J, Child S, Halford J, Boyland E. Children’s exposure to food advertising: the impact of statutory restrictions. Health Promotion International. 2017 Oct 30.
18. Palmedo PC, Dorfman L, Garza S, Murphy E, Freudenberg N. Countermarketing alcohol and unhealthy food: An effective strategy for preventing noncommunicable diseases? Lessons from tobacco. Annual Review of Public Health. 2017 Mar 20;38:119-44.
19. Mooney P. Too big to feed: Exploring the impacts of mega-mergers, consolidation and concentration of power in the agri-food sector. IPES-Food. 2017.
20. Johnston LM, Finegood DT. Cross-sector partnerships and public health: challenges and opportunities for addressing obesity and noncommunicable diseases through engagement with the private sector. Annual Review of Public Health. 2015 Mar 18;36:255-71.
21. See for example: Galea G, McKee M. Public–private partnerships with large corporations: setting the ground rules for better health. Health Policy. 2014 Apr 1;115(2-3):138-40; Knai C, Petticrew M, Durand MA, Eastmure E, James L, Mehrotra A, Scott C, Mays N. Has a public–private partnership resulted in action on healthier diets in England? An analysis of the Public Health Responsibility Deal food pledges. Food Policy. 2015 Jul 1;54:1; Bryden A, Petticrew M, Mays N, Eastmure E, Knai C. Voluntary agreements between government and business—a scoping review of the literature with specific reference to the Public Health Responsibility Deal. Health Policy. 2013 May 1;110(2-3):186-97; Swinburn B, Kraak V, Rutter H, Vandevijvere S, Lobstein T, Sacks G, Gomes F, Marsh T, Magnusson R. Strengthening of accountability systems to create healthy food environments and reduce global obesity. The Lancet. 2015;385(9986):2534-45.
22. New York City Department of Health and Mental Hygiene. Preventing Non-Communicable Diseases and Injuries Innovative Solutions from New York City, 2011.
23. Nestle M. Food Politics: How the Food Industry Influences Nutrition and Health. University of California Press, 2003.
24. Centers for Disease Control and Prevention (CDC). Ten great public health achievements–United States, 1900-1999. MMWR. Morbidity and Mortality Weekly Report. 1999;48(12):241.